Personal health is complex. It’s not only affected by an individual’s genetics, characteristics and behavior; it’s also affected by many factors out of a person’s control, like where they are born, live and work. These social determinants of health (SDOH) can hugely impact health outcomes. In fact, one study by the ASPE estimated that, on average, clinical care impacts only 20 percent of county-level variation in health outcomes, while SDOH affect as much as 50 percent of health outcomes. That’s why it’s important to identify them for each patient and provide helpful resources as needed.
Here are a few ways you can use technology in the office to screen for SDOH and help everyone live their healthiest lives.
Get to know your patients and their communities
Even though SDOH impact someone’s health and the care they require, a study by the JAMA Network found that only 24% of hospitals and 16% of physician practices screened for food insecurity, utility needs, transportation needs, housing instability and interpersonal violence. Patients often don’t realize these environmental factors influence their health, so they easily go unaddressed unless prompted by a healthcare provider.
Screening for SDOH should be a part of your rooming process, if it’s not already. This is a mandatory requirement for several hospitals and practices, but many are still not doing this because of limited resources. To start, make sure your clinical staff has a base understanding of the communities in which they serve. Understanding the SDOH that are prominent in patients’ communities may increase provider empathy and lead them to ask more relevant questions in the exam room.
It’s important to keep in mind your team’s implicit biases while discussing surrounding communities. These unconscious attitudes toward others are difficult to acknowledge but can cause disparities in healthcare. Try challenging your employees to address their own implicit biases because overcoming these feelings is the only way to get truly equal care for all. A great tool to use is Harvard’s Implicit Association Test.
With this baseline of knowledge established, you can then devise a system for screening SDOH in each appointment so your clinical staff can get a better picture of each patient’s unique circumstances to adjust care accordingly and connect them with the appropriate support. To make this process efficient, link to SDOH forms on exam room devices and ask patients to fill them out while they wait for their doctor.
Connect patients with resources

But it’s not enough to simply collect the data. Doctors should use this data to gear the conversation and connect patients with resources that improve their health equity. In a recent interview with Dr. Kashyap Patel, the CEO of Carolina Blood and Cancer Care Associates and a full-time practicing oncologist, he said “I can’t sleep peacefully at night if I found out today in my office that 17 patients have food insecurity…if I identify patients sleeping on the street or in a car because they don’t have a home, then I have a moral imperative as well as a I would say a quality care imperative, to find a shelter.”
CMMI currently doesn’t reimburse practices for spending that extra time with patients, finding them the help they need, which can put a practice at financial risk—even as it improves the quality of care. However, Dr. Patel says, “Every committee in America has resources from communities. The issue is that because we are compartmentalized, fragmented and reductionist, we don’t assimilate these resources.”
One efficient way to help patients in need is to speak to your peers about the resources they recommend, and then link to these resources on your exam room devices. That way providers can text or email information from the devices directly to patients, rather than having to spend time printing it out.
Be accommodating
If your practice wants to go the extra mile to really address health disparities, you can make adjustments inside your practice to help everyone have a better patient experience. For example, if a percentage of patients don’t have a reliable mode of transportation or have a difficult time getting off work, consider offering open-access scheduling, evening and weekend hours or telehealth services.
Whether or not you have a large Spanish-speaking population, it’s always a good idea to have processes in place to help patients whose first language is not English. This could include having education available in the waiting room and exam room for multiple languages. Imagery, such as infographics and 3D anatomicals on an exam room touchscreen, are also helpful since they don’t rely on written words.
There are some SDOH that practice adjustments unfortunately can’t account for, but that’s where the community resources come in. Don’t assume patients are aware of the assistance programs they qualify for and how to access them. Remind your clinical staff to discuss these when relevant in the exam room and send the information home with patients. If there’s a resource or service you want all patients to be aware of, you can inform patients via a waiting room device that will display that information alongside relevant education.
Improve health literacy to improve health outcomes
Health literacy is an issue for patients in general, not just those affected by SDOH. The CDC states that 9 out of 10 U.S. adults struggle to understand health information. People with poor literacy levels are shown to be less responsive to health education and keeping up with their treatment plans. To have the most success at providing health equity, it’s important to develop a strategy for improving health literacy alongside your efforts to address SDOH.
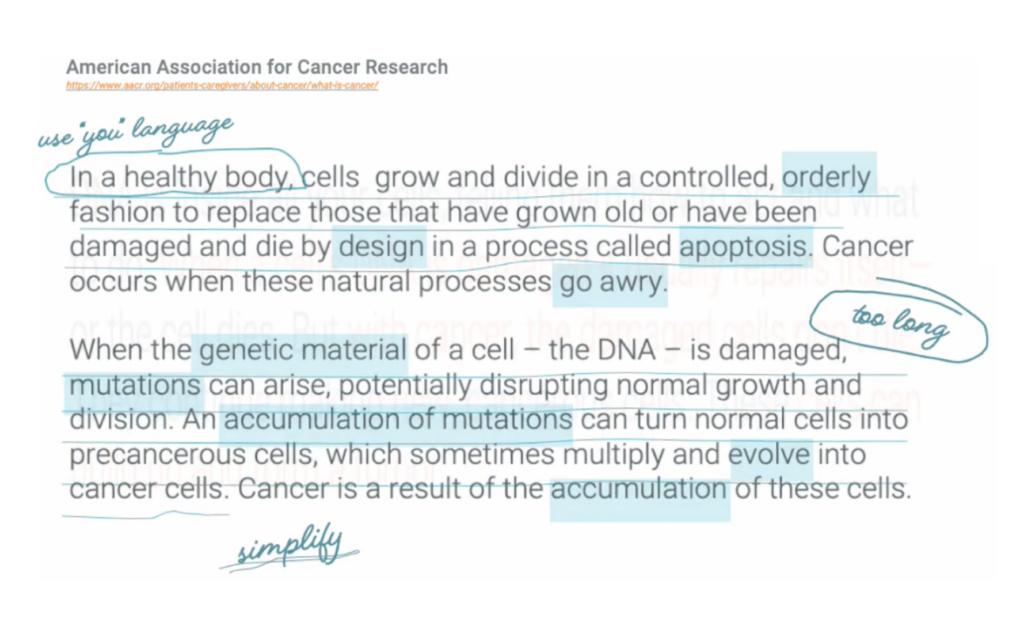
In a survey commissioned with market research leader OnePoll, 54% of respondents were afraid to ask their healthcare provider about their health condition/symptoms because they were concerned that they wouldn’t be able to understand the terminology their healthcare provider used when answering questions. Patients don’t respond well to medical jargon. They need easy-to-understand education in plain language that they can act on. Keep this in mind when choosing waiting room and exam room education tools and encourage your clinical staff to also use simple language when speaking to patients. Healthcare providers can also practice the teach-back method to verify that the patient understands their diagnosis and next steps.
Ready to start implementing these recommendations into your practice? Check out solutions for educating patients and screening for SDOH in our patient engagement platform.

